Allergy to Chemicals caused my Dermatitis
A 39-year-old woman developed asthma from jewelry cleaning lotion she used in her trade. A jeweler developed contact dermatitis from the sulfuric acid he used as a cleaning agent. He had to wear gloves all the time because both his hands had deep wounds.
“If conditions such as Eczema/Dermatitis are suppressed with Steroid creams instead of being properly treated, the Eczema/Dermatitis can gravitate to the lungs and manifest later as Asthma and many other diseases”
What is Dermatitis?

Dermatitis is an inflammation of the skin. The word “dermatitis” is used to describe a number of different skin rashes that are caused by infections, allergies, and irritating substances.
Most Common Types of Dermatitis
1. Atopic Dermatitis
Is a condition that causes itchy, inflamed skin. It typically affects the insides of the elbows, backs of the knees, and the face, but can cover most of the body. Atopic dermatitis falls into a category of diseases called atopic, a term originally used to describe the allergic conditions of asthma and hay fever. People who live in urban areas and in climates with low humidity seem to be at an increased risk for developing atopic dermatitis.
What are the Causes of Atopic Dermatitis
Atopic dermatitis is due to a skin reaction (similar to an allergy) in the skin. The reaction leads to ongoing swelling and redness. People with atopic dermatitis may be more sensitive because their skin lacks certain proteins.
Atopic dermatitis is most common in infants. It may start as early as age 2 to 6 months. Many people outgrow it by early adulthood. People with atopic dermatitis often have asthma or seasonal allergies. There is often a family history of allergies such as asthma, hay fever, or eczema. People with atopic dermatitis often test positive to allergy skin tests.
The following can make atopic dermatitis symptoms worse:
- Allergies to pollen, mould, dust mites, or animals
- Cold and dry air in the winter
- Colds or the flu
- Contact with irritants and chemicals
- Contact with rough materials, such as wool
- Dry skin
- Emotional stress
- Drying out of the skin from taking frequent baths or showers and swimming very often
- Getting too hot or too cold, as well as sudden changes in temperature
- Perfumes or dyes added to skin lotions or soaps
What are the symptoms of atopic dermatitis?
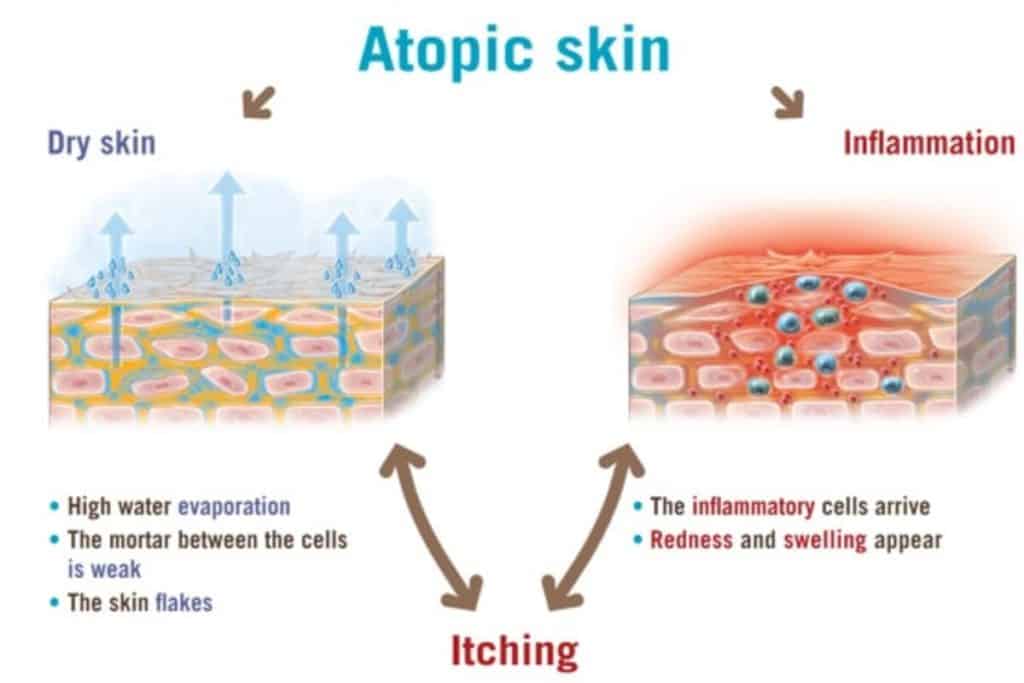
The primary symptom of atopic dermatitis is dry, itchy skin that often turns into a red rash. During a flare, atopic dermatitis becomes a red, itchy rash. Many different physical and internal factors can trigger an eczema flare-up. The resulting inflammation causes increased blood flow and the urge to itch.
Eczema flares are part of the agonizing itch-scratch cycle. It’s hard to fight the physical and psychological components that drive the itch-scratch cycle. Scratching feels good at the time but can lead to more inflammation and even skin infections.
Atopic dermatitis presents different symptoms depending on a person’s age.
Symptoms in infants can include:

- dry, itchy, scaly skin
- a rash on the scalp or cheeks
- a rash that may bubble and weep clear fluid
Infants with these symptoms may have trouble sleeping due to itchy skin. Infants with atopic dermatitis may also develop skin infections from scratching.
Symptoms in children can include:

- a rash in the creases of the elbows, knees, or both
- scaly patches of skin at the site of the rash
- lightened or darkened skin spots
- thick, leathery skin
- extremely dry and scaly skin
- rashes on the neck and face, especially around the eyes
Symptoms in adults can include:
Adults who had atopic dermatitis as children may have discoloured skin that is easily irritated.
Who Gets Atopic Dermatitis?
Atopic dermatitis is most common in babies and children. But it can happen to anyone. People who live in cities and dry climates may be more likely to get this disease.
When children with atopic dermatitis grow older, this problem can improve or go away. But the skin may stay dry and easy to irritate. At other times, atopic dermatitis is a problem in adulthood.
You can’t “catch” the disease or give it to other people.
Treatments and drugs
Medications
- Creams that control itching and inflammation. Your doctor may prescribe a corticosteroid cream or ointment. Talk with your doctor before using any topical corticosteroid. Overuse of this drug may cause skin irritation or discolouration, thinning of the skin, infections, and stretch marks.
- Creams that help repair the skin. Drugs called calcineurin inhibitors — such as tacrolimus (Protopic) and pimecrolimus (Elidel) — affect your immune system. Applied to the skin, they help maintain normal skin, control itching and reduce flares of atopic dermatitis. Due to possible side effects, these prescription-only drugs are used only when other treatments have failed or if someone can’t tolerate other treatments. They are approved for children older than 2 and for adults.
- Drugs to fight infection. You may need antibiotics if you have a bacterial skin infection or an open sore or cracked skin caused by scratching. Your doctor may recommend taking oral antibiotics for a short time to treat an infection. Or he or she may suggest you take it for a longer time to reduce bacteria on your skin and to prevent another infection.
- Oral anti-itch drugs. If itching is severe, oral antihistamines may help. Diphenhydramine (Benadryl, others) can make you sleepy and may be especially helpful at bedtime.
- Oral or injected drugs that control inflammation. For more severe cases, your doctor may prescribe oral corticosteroids — such as prednisone — or an injected corticosteroid. These drugs are effective but can’t be used long term because of potentially serious side effects. Continue moisturizing and using other self-care remedies to prevent a flare-up after you stop taking the corticosteroids.
Therapies
- Wet dressings. An effective, intensive treatment for severe atopic dermatitis involves wrapping the affected area with topical corticosteroids and wet bandages. It has proven to control signs and symptoms within hours to days. Sometimes it is done in a hospital because it’s labour intensive and requires nursing expertise. Or, ask your doctor about learning how to do this technique at home.
- Light therapy. The simplest form of light therapy (phototherapy) involves exposing your skin to controlled amounts of natural sunlight. Other forms use artificial ultraviolet A (UVA) and narrowband UVB either alone or with medications. Though effective, long-term light therapy has harmful effects, including premature skin ageing and an increased risk of skin cancer. For these reasons, phototherapy is not used for infants and young children. Talk to your doctor about the pros and cons of light therapy in your situation.
- Treatment for stress. Counselling may help children and young adults who are extremely embarrassed or frustrated by their skin condition.
- Relaxation, behaviour modification or biofeedback. These approaches may help you with habitual scratching.
2. Contact Dermatitis

When your skin comes into contact with the substance in the environment that you are allergic to, it may react by causing your skin to itch and become red. This is called contact dermatitis.
Allergic Reaction Triggers
If it’s an allergy, your immune system is involved. After you touch something, it mistakenly thinks your body is under attack. It springs into action, making antibodies to fight the invader. A chain of events causes a release of chemicals, including histamine. That’s what causes the allergic reaction — in this case, an itchy rash. It’s called allergic contact dermatitis.
Common triggers for contact dermatitis are:
- Poison ivy, poison oak, and poison sumac
- Hair dyes or straighteners
- Jewellery
- Nickel, a metal found in jewellery and belt buckles
- Leather (specifically, chemicals used in tanning leather)
- Latex rubber
- Citrus fruit, especially the peel
- Fragrances in soaps, shampoos, lotions, perfumes, and cosmetics
- Some medications you put on your skin
Usually, you won’t get a rash the first time your skin touches something you’re allergic to. But that touch sensitizes your skin, and you could have a reaction the next time. If you got a rash on first contact, chances are you’ve touched that trigger before and just didn’t know it.
Symptoms of contact dermatitis include:
- Red, irritated skin
- Itching
- Swelling
- Bumps or blisters, sometimes filled with clear fluid
- Hot or tender skin
These symptoms can range from mild to severe, and they can appear anywhere from a few hours to 10 days after coming into contact with the irritant or allergen. A contact dermatitis rash cannot be spread to anyone else.
If you’ve come into contact with a potential allergen or irritant, immediately wash the affected area with soap and water.
Treatment for Contact Dermatitis
Treatment is the same for both types of contact dermatitis.
Avoid what is causing your rash. If avoiding the cause will be difficult, ask your dermatologist for help.
For example, if you are allergic to latex but must wear exam gloves, your dermatologist can recommend another type of glove that you can wear. If you must work outdoors where poison ivy grows, your dermatologist can recommend a protective barrier cream and clothing that can help.Treat the rash. Once you can avoid the cause, your rash should clear. To relieve your symptoms, a dermatologist may recommend the following:
- Mild reaction: Antihistamine pills, moisturizer, and a corticosteroid that you can apply to your skin. Most patients apply for medicine twice a day for 1 week and once a day for 1 to 2 weeks. Oatmeal baths can relieve discomfort.
- Severe reaction: If you have a lot of swelling, your face swells, or the rash covers much of your body, you may need a strong medication. Your dermatologist may prescribe prednisone. It is important to take this medication exactly as directed to avoid another flare. Wet dressings can help soothe skin that has lots of oozing and crusting. If your dermatologist recommends wet dressings, you’ll receive instructions to help you make these at home.
3. Neurodermatitis

Neurodermatitis is a skin condition that starts with a patch of itchy skin. Scratching makes it even itchier. This itch-scratch cycle causes the affected skin to become thick and leathery. You may develop several itchy spots, typically on the neck, wrist, forearm, thigh or ankle.
Neurodermatitis — also known as lichen simplex chronicus — is not life-threatening or contagious. But the itching can be so intense or recurrent that it disrupts your sleep, sexual function and quality of life.
What are the causes of Neurodermatitis?
Scientists have yet to find the exact cause of this problem, however, there are a number of trigger points that have been associated with the lichen simplex chronicus condition, this includes:
- Clothing is worn tightly and made of synthetic fabric or wool
- Dry skin
- These triggers are less frequent but could result in a neurodermatitis attack
- Exhaust from traffic (long-term exposure)
- Exposure to allergens and skin irritants (i.e.hair sprays or dyes)
- Heat exposure
- Insect Bites
- Prolonged periods of intense stress or emotional trauma
- Lack of adequate blood flow or poor circulation
- Keloid Scars
Symptoms of Neurodermatitis
Signs and symptoms of neurodermatitis include:
- An itchy skin patch or patches
- The leathery or scaly texture on the affected areas
- A raised, rough patch or patches that are red or darker than the rest of your skin
The condition involves areas that can be reached for scratching — the head, neck, wrist, forearm, ankle, vulva, scrotum or anus. The itchiness, which can be intense, may come and go or be nonstop. You may scratch out of habit and while sleeping.
Neurodermatitis Treatment
Because this condition is accompanied by excessive itching and scratching, the objective of treatment is to eliminate this reaction. The following are known treatments that have been prescribed by a physician:
1. Topical corticosteroid to reduce inflammation and alleviate the itch.
2. Topical antibiotics can fight infection in the event a breakage of the skin has occurred from the scratching.
3. An oral antibiotic is a more powerful medication to eliminate any secondary infection.
4. Topical keratolytic is a preparation containing urea, salicylic acid, or lactic acid that can help in the reduction of thick skin.
In severe cases, doctors have prescribed a sedative or tranquillizer. This is used in cases of severe anxiety to induce sleep.
4. Stasis Dermatitis

Stasis dermatitis is a skin condition that develops in people with poor circulation. It typically occurs in the lower legs. In serious cases, stasis dermatitis can progress into ulcers.
Common Causes of Stasis Dermatitis
Poor circulation causes stasis dermatitis. Typically, poor circulation is the result of a chronic, or long-term, the condition called venous insufficiency. Venous insufficiency occurs when your veins have trouble sending blood to your heart. There are one-way valves inside your leg veins that keep your blood flowing in the right direction, which is toward your heart.
In people with venous insufficiency, these valves become weak. This allows blood to flow back toward the feet and pool in your legs instead of continuing to flow toward your heart. This pooling of blood is what causes stasis dermatitis.
Varicose veins and congestive heart failure are also known causes of leg swelling and stasis dermatitis.
Most of the conditions that cause stasis dermatitis usually develop in people as they get older. However, there are also several causes that are unrelated to age, including:
- surgery, such as using a leg vein for bypass surgery
- deep vein thrombosis in your leg
- traumatic injury to your lower legs
Stasis Dermatitis Symptoms
Stasis Dermatitis affects the legs of a person. Naturally, the symptoms of this disease are mainly visible in the legs of the sufferer. But it can also affect other body parts like the arms if they suffer from poor blood circulation. The symptoms include :
- The appearance of red rashes
- Itching in the affected area
- Accumulation of fluids under the weakened skin region
- Darkening or thickening of the skin in the ankles or legs
- Development of ulcers and sores in the weak skin area
- Pain in the legs
- Cracks in the affected region of the skin
- Thickened skin in the affected leg region
- Formation of lesions in the legs
Stasis Dermatitis Treatment
There are several things you can do at home to treat stasis dermatitis. You should:
- avoid standing and sitting for long periods of time
- prop up your feet when sitting
- wear compression stockings
- wear loose-fitting clothing to avoid irritating your skin
Ask your doctor about the types of skin creams and ointments you can use. You should avoid using the following products:
- lanolin
- calamine and other lotions that dry your skin
- topical antibiotic ointments such a neomycin
- benzocaine and other numbing medications
5. Seborrheic Dermatitis

Seborrheic dermatitis, also known as seborrheic eczema or simply as seborrhea, is a chronic, relapsing and usually mild dermatitis. In infants, seborrheic dermatitis is called cradle cap. Dandruff is a type of seborrheic dermatitis where inflammation is not present. Seborrheic dermatitis is a skin disorder affecting the scalp, face, and torso.
Causes of Seborrheic Dermatitis
Although the cause is unknown, several contributing factors may play a role in developing seborrheic dermatitis: abnormality of the oil glands and hair follicles, a yeast fungus with bacteria growing in the sebum, production of certain hormones, stress, change of seasons (outbreaks seem worse in winter) and fatigue.
Seborrheic Dermatitis Symptoms
Seborrheic dermatitis symptoms include:
- Skin flakes (dandruff) on your scalp, hair, eyebrows, beard or moustache
- Patches of greasy skin covered with flaky white or yellow scales or crust on the scalp, ears, face, chest, armpits, scrotum or other parts of the body
- Red skin
- Redness or crusting of the eyelids (blepharitis)
- Possibly itching or stinging
Treatment for seborrheic dermatitis
Treatment of hair-bearing areas, like the scalp, often includes the use of a shampoo that may contain one or more of the following ingredients:
- Tar
- Antifungal antibiotic
- Zinc pyrithione
- Selenium sulfide
In addition, the application of a topical steroid lotion or solution of weak to moderate potency is effective such as desonide (Desonate, DesOwen, LoKara, Verdeso), betamethasone valerate (Valisone), hydrocortisone, and 0.025% triamcinolone (Aristocort, Aristocort HP, Kenalog, Triderm).
For non-hair-bearing areas, the application of a weak to moderately potent topical steroid or topical antifungal cream is frequently effective. The use of tacrolimus (Protopic) or pimecrolimus (Elidel) ointments can be effective but is quite an expensive alternative.
It needs to be stressed that since this condition is incurable but easily controllable; if the disease is active and the treatment is stopped, one should expect seborrheic dermatitis to recur. One should also use effective medications just enough to control the symptoms. Excessive treatment of apparently normal skin is economically wasteful as well as potentially risky.
HOW WE TREAT DERMATITIS
With us, we get to the root of the problem, identifying and eliminating the allergen that is causing the recurring symptoms.
We offer the prospect of relief to those who suffer from addiction and allergies by reprogramming the brain to perfect health. Just like rebooting a computer, we can reboot our nervous system to overcome the adverse reactions of brain and body.
To fully understand what we do, one needs to know some Oriental medical principles. We take the acupuncture and Oriental medical theories and developed a technique that can eliminate the reaction from the root.
Addictions can definitely cause illness. Continuous contact with an allergen produces toxins in the body and causes blockages in the meridians. If these blockages are not cleared, reactions to the allergens often produce symptoms that mimic other diseases.

By clearing all your environmental, heavy metal and food allergies from the protocol, we strengthen the immune system, improve digestion and absorption. This allows the body to get the necessary nutrients, which are essential for life. without causing any reactions.
One allergen is cleared per visit. Each individual has a different genetic makeup and health history so the number of sessions required varies from one individual to another. For some people, allergens are cleared immediately however, for others it may take many sessions to accomplish the desired results.
Some people might raise their eyebrows and ask, “Can you really eliminate my Dermatitis?” We answer with a resounding “YES!”
46 YEARS OF DERMATITIS CLEARED BY NAET
A man, who suffered the first attack of dermatitis at the age of five, did not consult any allergist until he was 46. By that time his entire body was covered with atopic dermatitis, which had become chronic and had so thickened and distorted the skin that the scars are likely to be permanent. During this 40-year period, eczema had gradually spread over the entire body and was complicated by hay fever and asthma.
Unlike some cases of childhood dermatitis, his symptoms did not decrease as he entered puberty. They remained present at all times and gradually increased in intensity.
When he finally consulted an allergist, he was tested and found to be sensitive to a number of foods, pollen, and other inhalants (animal epithelial, pollens, dust) as well as the medicines he was using for internal and external application.
After he tried traditional allergy treatments without positive results, he came to our office. He was treated for various food allergies, fabrics, and environmental substances and showed marked improvements in his condition. However, the scars were so deep and of such long duration that his skin will probably no return to a normal state for years, even though he is absolutely asymptomatic. This is an example of neglected symptoms that are nearly impossible to correct.
Had this patient consulted an allergist and received proper allergic treatment before dermatitis became so severe, it would have cleared up entirely, without leaving any scars.
Poison ivy and poison oak are both classic examples of allergens that can cause contact dermatitis. The response to these plants is a true allergy, since not everyone reacts to them, and many times prolonged contact does not bring allergic reactions. In other individuals, one contact is sufficient to sensitize them.
Connect with us through our Facebook page at www.facebook.com/NAETDubai or visit: www.naetdubai.com. You will find a wealth of information here along with an opportunity to speak confidentially through WhatsApp 056-639 0197 or Phone Call 04-420 1633.
You may also email us at admin@naetdubai.com




4 Responses
Thank you for your comment ???? . Please don’t forget to subscribe to our blog and you will receive mails once we published new blogs. Feel free to contact us if you need any further information. Cheers!
Thank you for your comment.Please dont forget to subscribe to our blog and feel free to contact us for any further details.
Thank you so much for your comment. Please don’t forget to subscribe to our blogs. Feel free to contact us if you need any further information.
Not only the articles are excellent but NAET is. It healed my histamin. fructose, apple, eggs, pet hair allergy. It changed my life completely. Give it a try … it is worth to do it. Don’t suffer for the next years.